Uterine scarring, also known as intrauterine adhesions or Asherman’s syndrome, is characterised by scar tissue within the uterine cavity. These adhesions can result in a variety of symptoms and complications, including abnormal menstrual bleeding, infertility, and recurrent miscarriages.
Exploring the underlying causes and risk factors associated with uterine scarring, including prior uterine surgeries, provides valuable insights into understanding and managing this condition. In this essay, we will delve into the various factors that contribute to uterine scarring, with a particular focus on the role of prior uterine surgeries.
Introduction to Uterine Scarring
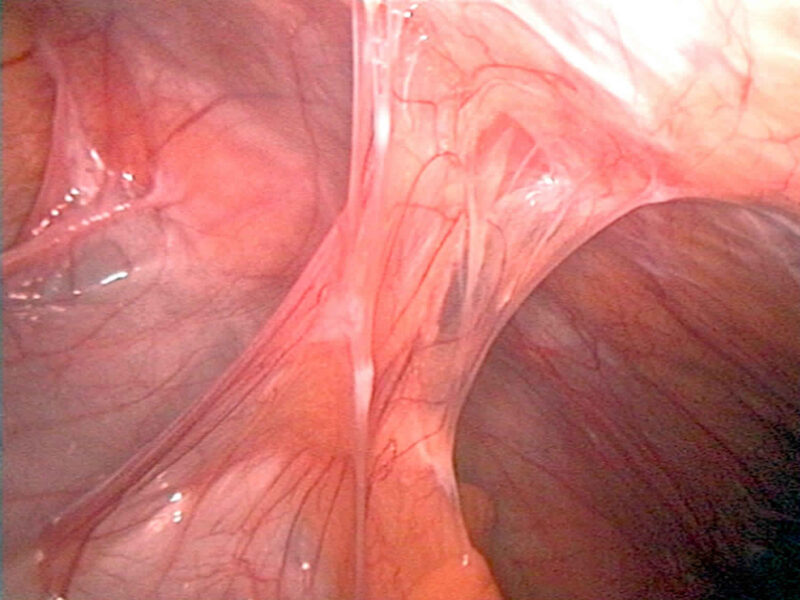
Uterine scarring occurs when scar tissue forms within the uterine cavity, leading to adhesions that can interfere with normal uterine function. These adhesions can vary in severity, ranging from thin filmy bands to dense, fibrous scar tissue.
Uterine scarring is commonly associated with a history of uterine surgeries, but other factors can also contribute to its development.
Underlying Causes of Uterine Scarring
Uterine Surgeries

- Prior uterine surgeries, such as dilation and curettage (D&C), cesarean section (C-section), myomectomy (removal of uterine fibroids), or uterine polyp removal, are significant risk factors for uterine scarring.
- These surgical procedures can cause trauma to the endometrium (the inner lining of the uterus), leading to inadequate healing and the formation of scar tissue.
Infections
- Uterine infections, such as endometritis (inflammation of the endometrium) or pelvic inflammatory disease (PID), can increase the risk of uterine scarring.
- Infections can cause inflammation and damage to the endometrium, impairing its ability to heal properly and leading to the formation of adhesions.
Miscarriages or Pregnancy Complications
- Miscarriages, particularly those associated with retained products of conception, can increase the risk of uterine scarring.
- Pregnancy complications such as placental abruption, uterine rupture, or postpartum haemorrhage can also cause trauma to the uterine lining and contribute to scarring.
Endometrial Ablation
- Endometrial ablation procedures, used to treat heavy menstrual bleeding, involve the destruction or removal of the endometrial lining.
- While effective in reducing menstrual bleeding, endometrial ablation can also damage the endometrium and increase the risk of uterine scarring.
Role of Prior Uterine Surgeries
Dilation and Curettage (D&C):
- D&C procedures, performed to remove uterine tissue following a miscarriage, abortion, or to diagnose or treat certain gynaecological conditions, can cause trauma to the endometrium.
- Inadequate healing of the endometrial lining following D&C can lead to the formation of scar tissue and intrauterine adhesions.
Cesarean Section (C-Section):
- Cesarean deliveries involve surgical incisions in the uterus to deliver the baby, which can result in scarring and adhesion formation.
- In some cases, adhesions may form between the uterine wall and adjacent structures, such as the bladder or abdominal organs, leading to complications such as bowel obstruction or bladder injury.
Myomectomy
- Myomectomy procedures, performed to remove uterine fibroids while preserving the uterus, can also increase the risk of uterine scarring.
- Surgical manipulation of the uterine tissue during myomectomy can disrupt the endometrial lining and impair healing, resulting in the formation of scar tissue.
Other Risk Factors for Uterine Scarring:
- Advanced Maternal Age: Women of advanced maternal age (typically defined as age 35 or older) may be at increased risk of uterine scarring due to age-related changes in the endometrium and decreased regenerative capacity.
- Recurrent Pregnancy Loss: Women with a history of recurrent miscarriages or pregnancy losses may have a higher likelihood of uterine scarring, particularly if retained products of conception are present following miscarriage.
- Uncontrolled Endometrial Inflammation: Chronic inflammatory conditions affecting the endometrium, such as endometriosis or chronic endometritis, can impair the healing process and predispose to scar tissue formation.
Conclusion:
Uterine scarring is a complex condition influenced by various factors, including prior uterine surgeries, infections, pregnancy complications, and maternal age. Understanding the underlying causes and risk factors associated with uterine scarring is essential for early detection, diagnosis, and management of this condition.
While prior uterine surgeries, such as D&C, C-section, and myomectomy, are significant contributors to uterine scarring, other factors such as infections and pregnancy complications also play a role.
By identifying individuals at risk and implementing preventive measures, healthcare providers can help minimize the incidence and severity of uterine scarring, ultimately improving reproductive outcomes and women’s health.
Related Tags
Taiwo Olawuyi
Taiwo Olawuyi is a highly dedicated and passionate professional blogger, renowned for her ability to create captivating, informative, and engaging content in the realm of health and wellness. She holds a Bachelor's degree in Political Science from Olabisi Onabanjo University and a Master's degree in Adult Education from the prestigious University of Ibadan. Her profound passion for health and wellness, coupled with her unwavering dedication to her audience, serves as a constant source of inspiration and enlightenment for readers worldwide.