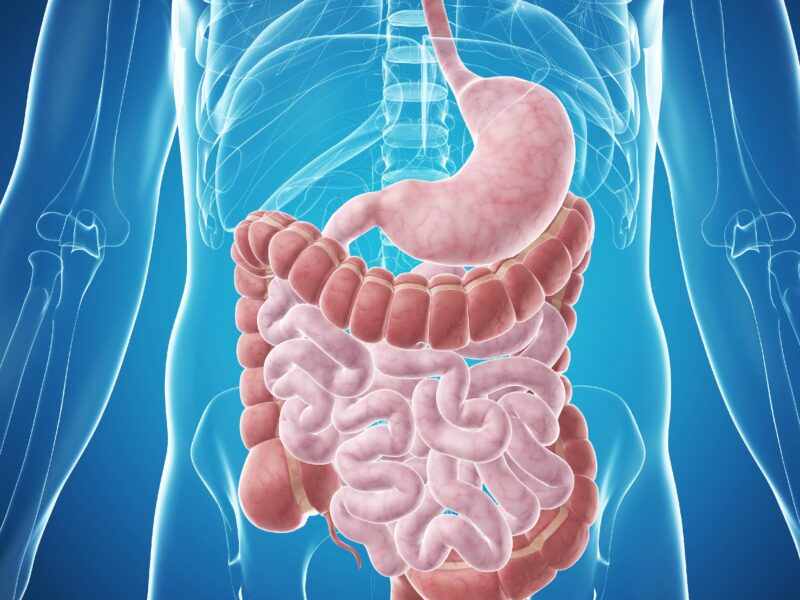
Digestive disorders affecting the intestine encompass many conditions that can significantly impact an individual’s quality of life. From irritable bowel syndrome (IBS) to inflammatory bowel disease (IBD), including Crohn’s disease and ulcerative colitis, as well as celiac disease and diverticulitis, these disorders present diverse challenges in diagnosis and management.
This comprehensive exploration will delve into the symptoms, causes, diagnosis, and management of these common digestive disorders, along with their impact on patients’ overall well-being.
Irritable Bowel Syndrome (IBS)
Irritable bowel syndrome (IBS) is a common gastrointestinal disorder characterised by abdominal pain, bloating, and changes in bowel habits without evidence of structural abnormalities.
The exact cause of IBS remains unclear, but factors such as altered gut motility, visceral hypersensitivity, intestinal inflammation, and dysregulated gut-brain axis may contribute to its development. Diagnosis of IBS is based on clinical symptoms and exclusion of other conditions. Management strategies include dietary modifications, stress management, lifestyle changes, and medications to alleviate symptoms and improve quality of life.
Inflammatory Bowel Disease (IBD)

Inflammatory bowel disease (IBD) encompasses two primary conditions: Crohn’s disease and ulcerative colitis, both of which involve chronic inflammation of the gastrointestinal tract. Crohn’s disease can affect any part of the digestive tract, from the mouth to the anus, and is characterised by transmural inflammation and discontinuous lesions.
Ulcerative colitis primarily affects the colon and rectum, causing continuous mucosal inflammation and ulceration. The exact aetiology of IBD is multifactorial, involving genetic predisposition, immune dysregulation, environmental triggers, and alterations in the gut microbiome.
Diagnosis relies on clinical evaluation, endoscopic findings, histopathological examination, and imaging studies. Treatment aims to induce and maintain remission, reduce inflammation, and prevent complications through medication, dietary modifications, surgery, and lifestyle interventions.
Celiac Disease
Celiac disease is an autoimmune disorder characterized by an immune reaction to gluten, a protein found in wheat, barley, and rye. In individuals with celiac disease, ingestion of gluten triggers an inflammatory response in the small intestine, leading to damage to the intestinal lining and malabsorption of nutrients.
Genetic predisposition, gluten consumption, and environmental factors contribute to the development of celiac disease. Diagnosis is based on serological tests for specific antibodies and confirmation by intestinal biopsy. Treatment involves strict adherence to a gluten-free diet to alleviate symptoms, promote intestinal healing, and prevent long-term complications such as malnutrition, osteoporosis, and other autoimmune disorders.
Diverticulitis
Diverticulitis is a condition characterized by inflammation or infection of the diverticula, small pouches that form in the wall of the colon. Diverticulitis often occurs in individuals with diverticulosis, a common age-related condition characterized by the presence of diverticula.
The exact cause of diverticulitis is unclear, but factors such as age, a diet low in fibre, obesity, and physical inactivity may contribute to its development. Diagnosis is based on clinical symptoms, physical examination, laboratory tests, and imaging studies.
Management involves antibiotic therapy, dietary modifications (such as a high-fibre diet), pain management, and, in severe cases, hospitalization and surgical intervention.
Impact on Patients’ Quality of Life
Digestive disorders affecting the intestine can have a profound impact on patients’ physical, emotional, and social well-being. Chronic symptoms such as abdominal pain, diarrhoea, constipation, bloating, and fatigue can significantly impair daily activities, work productivity, social interactions, and mental health.
Patients may experience anxiety, depression, social isolation, and reduced quality of life due to the unpredictable nature of their symptoms and the stigma associated with gastrointestinal disorders. Moreover, the burden of managing these conditions, including frequent medical visits, diagnostic tests, medication regimens, dietary restrictions, and lifestyle modifications, can further exacerbate the challenges faced by patients and their caregivers.
Conclusion
In conclusion, digestive disorders affecting the intestine encompass a diverse spectrum of conditions, each with its unique symptoms, causes, diagnosis, and management strategies. From functional gastrointestinal disorders such as IBS to chronic inflammatory conditions like IBD, celiac disease, and diverticulitis, these disorders present complex challenges in clinical practice and patient care.
Understanding the underlying mechanisms of these disorders, promoting early detection and diagnosis, and implementing multidisciplinary approaches to treatment and support are essential for optimizing outcomes and enhancing patients’ quality of life. Through ongoing research, education, and advocacy efforts, we can advance our understanding of these conditions and improve the lives of individuals affected by digestive disorders.
Related Tags
Taiwo Olawuyi
Taiwo Olawuyi is a highly dedicated and passionate professional blogger, renowned for her ability to create captivating, informative, and engaging content in the realm of health and wellness. She holds a Bachelor's degree in Political Science from Olabisi Onabanjo University and a Master's degree in Adult Education from the prestigious University of Ibadan. Her profound passion for health and wellness, coupled with her unwavering dedication to her audience, serves as a constant source of inspiration and enlightenment for readers worldwide.